
I have struggled to get my head around the effect of ecosystems within the healthcare system; it is so complex.
In recent weeks, I have recognized the barriers and opportunities around the challenges of building ecosystems for health services to deliver real change within our healthcare and its management.
To help me, I have found some excellent observations to gain this deeper appreciation of the complexities involved. The links are shown at the bottom of this post.
This is my opening summary to relate my understanding of how ecosystem designs might help change this vital sector of our economies.
The first starting point is that the patient themselves have to become the centre of any future healthcare system, based on ecosystem solutions. Why? Firstly, the patient or customer will increasingly be demanding and expecting personalized treatment and want to be able to shop around to achieve this. Secondly, they are expecting and wanting to be part of a controlled method and choose advice and care delivery more than ever. Thirdly, they will shop for quality and cost as the cost models will increasingly look for this personalization to determine the premiums. The final customer will be central to drive the change, and the providers of ‘services’ keen to reposition themselves as responsive to this ‘need.’
The essential debate is what is needed in health service to change and prepare to pay.
One of the main ‘intents of change’ will be realizing the potential that ‘we’ are not forced to buy a ‘blanket’ cover as the primary solution on offer. Tailoring for individuals offers a very different value proposition potential. The patient, the premium payer, are increasingly expecting and demanding higher levels of personalized service. Equally, the services providers can see this as the ‘way forward’ to tailor services and costs incurred to those actually using their services to gain different competitive advantage points and, more radically, looking at rewarding those that do not, with different value proposition points.
The challenge to overcome is the ability to connect the essential parts of the health ecosystem to realize this, to ‘talk to each other by exchanging the critical parts of a complex story. To get to this point will take an awful lot of connecting up and collaboration. Is this a reality or a pipe dream? Will this deliver better health services? What is really needed to offer personalized services, and are they economically viable? To undergo this understanding, there will be a lot of exploring and experimenting to assess new value propositions as the health ecosystem is so complex, it will be an evolving process of discovery, adjustment, and advancement. All parties need to become involved in learning and experimenting, understanding new value propositions for all involved in these ‘connected’ relationships.
This shift equally has a huge social implication that will have a real impact on each of us, where significantly improved service becomes essential and reflected in the premiums we expect to pay. Will it be more inclusive or more exclusive for those able to pay? It is recognized increasingly that it will incur massive changes in health business models to adapt to this. Will society embrace this change? What will trigger this? Will movement occur by natural evolutionary design or based on finally addressing the growing health funding crisis found in most societies because it simply has to change?
To build the total ecosystem of heath will require this ‘block by building block’ process, learn from each other the value of connecting, seek out the value creation points, and adapt progressively towards these. It will certainly take sustaining investment and dedicated effort over several years by all involved, seeking new health value models.
To achieve any change understanding, we need to see a more open era of information sharing in healthcare.
This will increasingly come from the platforms that form around and combine all parties involved; made up of providers of service, the payers of our claims and costs, the pharma industry and medical profession, increasingly under pressure to tailor medical to our specific needs, and finally, we as the patients, looking for increasing transparency, responsiveness and convenience to get the best deals. That is demanding on all involved in any ecosystem to balance out the parties involved so all can realize a mutual value.
We also need to believe that any new system will drive efficiencies and effectiveness of service in better ways than we are experiencing today within our health services. We often hear of a host of unnecessary services, duplication, inefficient delivery of care, possible instances of fraud, all too often wasted spending, services often at inflated prices, the incurring of increasing and mounting administrative costs and burdens of regulatory controls, all struggling to inflame or tame this unwieldy beast. Will, it possibly change, can it?
This is where the idea or concept of ecosystems and platforms come in: driving new outcomes.
We know the drivers expected in outcomes, besides better services at lowering costs. These need to improve health behaviours as the incentive for premium reductions, the access to greater clinical choice, quality, and care. We want to see the bigger picture of the physical environment (the way we live) alongside the social and economic factors ‘kick in’ to prevent increasing sickness and raise social support and community engagement. Those are a big ask, but they become the real drivers of what we want from any health system to work towards. How we get from where we are to where we want our healthcare is a huge gap of opportunities and challenges. Getting everyone on the same page of successful outcomes is hard in itself. Far too many vested self-interests will hinder this need for change.
Enter the Ecosystem of Health – the digital, consumer-driven need.
There is increasing recognition within the healthcare industry, in all the payer, provider, life science and pharmaceutical industry, they will require new capabilities, leading to new business models. This will be a profound movement and impact across all those involved. The ability to rethink such a significant change will require a re-imagination of partners and how they interact with each other and with patients.
So we will see increasingly the emergence of multiple ecosystems within ecosystems that become more open, have a concept of mutuality both in formal and informal ways, that come together around shared goals, visions, ideals, standards and a new design that transforms healthcare. There is this incredible need for high levels of orchestration to realize this. The platform needs to coordinate interactions and collaborations among participants. A clear, explicit entity is set up to orchestrate so organizations can pursue different objectives to capture the value and deliver a significant user experience.
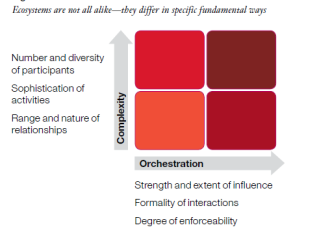
Ecosystems will not be alike; they will be precise on the task and design determined to ‘do the job’. I liked an IBM visual to give a nice overview of this.
Complexity will raise its head constantly.
Just image tackling such a healthcare system? Health is one of the most complex systems required to be tackled. I have been reading different views on this. This view offered by Chris Lawer, CEO of Umio, was well put in one of his excellent papers on transforming healthcare that captures much of the complexities within it:
“Complex problems in health such as these are notoriously difficult to address. Their root causes are multiple, tangled, hard to identify and impossible to extract from their effects. Attempts to resolve one problem can worsen another; they are dynamically linked and deeply nested.
Cost savings made in one part of a health system may incur bigger cost increases in another. Seeing, knowing and framing a complex problem is a challenge in itself as patients, practitioners, providers, and payers attach different meanings, contexts, priorities, values and assumptions to their importance, as well as how to solve them.
It is little wonder that efforts to resolve these complex dynamic health problems rarely succeed or meet their ambitions. Even the most breakthrough technological innovations suffer from slow or low adoption, contrary to high expectations. The much-promised digital transformation is only gradually coming. Change in health systems cannot be driven technologically alone. Whether drugs, apps, devices, or IT systems, many require too much effort to introduce, integrate with, or adapt existing practices or train teams; there is just too much to unlearn.
Often, their evidence is insufficiently compelling to persuade people to switch from long-established practices and systems. Clinicians and managers are reluctant to introduce risk, or they lack the time or inclination to change long-established routines. Each new intervention or innovation may even create inefficiency, to begin with, as users grapple with adoption. Often, payers simply cannot afford new drugs and devices or make the case to do so when faced with ever diminishing budgets that need to be expended on frontline services.
Despite the promise of rapid technological, medical and scientific advances, health spending is growing and is wasted whilst outcomes plateau or decline. Patients and professionals are increasingly dissatisfied whilst their expectations from new technologies and the media rise. Conflict and frustration mount whilst underlying disease, condition and problem root causes become more deep-seated and distant from view. The reality is that piecemeal adaptations and interventions are deepening system complexity further. The healthcare environment becomes overwhelmingly defined by crises, diverting actors’ attention from real possibilities for transformation and limiting their change efforts to incremental improvements or firefighting only. Time for a rethink.”
Chris believes current design thinking approaches in health suffer from what he has dubbed the 5S Syndrome:
Their problem framing scope is too narrow; they do not take a wide-enough systems view. They seek to understand problems in the context of solutions, which are too short-term and, more often than not, address symptoms rather than root causes.
His argument in moving forward and re-design health systems is that we need an apparent and distinctive separation of problem learning from solution design activity. This means, in Chris’s view, we must first frame those problems (or challenges/need) independent of the means to resolve them:
“This separation of problems (now opportunities) are easier to the theme, pivot, frame, analyze, compare, share and be assimilated by those tasked with designing value propositions and co-creating solutions, in his view.
He recommends we view health systems dynamically. These should be viewed through this ecosystem lens.
“It provides a new frame of reference for building problem learning, solution co-creation, adaptive strategy and leadership capabilities within care provider and industry organisations seeking to innovate, intervene and transform health ecosystems.”
Exploring the cutting edge of designing health care solutions through this ecosystem design application.
Chris Lawer, well for me, has provided some terrific insights to build this growing understanding of healthy ecosystems, in the complexities but also solutions to apply to the health industry, by looking consistently through this ecosystem lens (see links below). He offers some particular outcomes at growing collaborations through platform and ecosystem approaches in what he has been undertaking.
There is a growing body of work exploring this connecting up, including Aetna, United Healthcare, Cigna, Kaiser Permanente, Eli Lilly and Boehringer, as a few at the tip of the health industry iceberg of change to learn from.
The discovery of an exceptional report by Dave Chase
I loved one exceptional report by Dave Chase (@chasedave) of Cascadia, 94 pages reviewing the state of “the future health ecosystem today”, written in 2016 (link below). One comment I smiled over was, “the Swans are in the water, but what colour are they? As he states, “the healthcare industry is on the verge of its transistor moment” A really important “must go to” report to gain a detailed understanding of the complexity and emerging ecosystem solutions in health—a great learning deck.
The solid foundation of IBM put health ecosystems into context
In this short overview provided by IBM of how ecosystems and platforms are transforming health, I thought one visual, again by IBM, made a nice summary of the challenges as organizations seek ways to reinvent their business in the context of ecosystems in which they will have to find ways to participate.

Summary
The strategies will depend on the environment, the challenges that need to be addressed and the perceived value involved. The level of complexity is potentially as “wicked” as it can get. Complexity is not only in addressing the problem but visualizing the solutions. The more participants, the higher diversity of opinion and issues to be addressed, along with the application, investment and sophistication of those involved in the activities within the ecosystem, will be broad in design and specific in relationship needs. ‘Push back’ to change will be prevalent due to vested interests.
For me, addressing the health ecosystem will be about a long, hard, deeply committing journey for all those involved. The plus to encourage investment is that barriers to entry remain high in many areas of highly specialised service and can encourage change. There are formidable barriers for new entrants due to many highly scaled, entrenched and specialized positions.
Where real opportunity arises is for those who actively seize the platform and orchestration roles. These will determine the mechanisms for change and give this a certain robustness and enforcement. These orchestrating roles becomes the powerful catalyst. Here technology platform providers like Salesforce, Amazon, Google and many others will continue to enter the field, as it has a huge potential in extending their positioning. They can determine the type of experience to be delivered. If this is highly patient-centric, socially connected, it can be highly determined in a race to be a new winner in the health ecosystem movement.
****My thanks to different reports and papers to get myself even to this point.
To the IBM Institute of Business Value and its report “The new era of ecosystems”, Cascadia Capital LLC and the Dave Chase report “the future health ecosystem today” provided and finally, to Chris Lawer, the CEO of Umio-Health and his excellent views of blending ecosystem theory along with his organization’s practical application. In particular, in part of his post, I have quoted here, “Design thinking is struggling to transform healthcare: Here’s why“. Some amazing insights and reporting are shared on his company’s website.